What is a variant? An expert explains
Delta, Omicron, Alpha. Covid-19 variants keep appearing. But, what are variants? We asked Divya Shah, Epidemics Research Lead, to explain how variants happen, what they mean for treatments and vaccines – including for Covid-19 – and how we can prevent them.
Although the terms viral mutants, variants and strains are often used interchangeably, they generally hold different meanings.
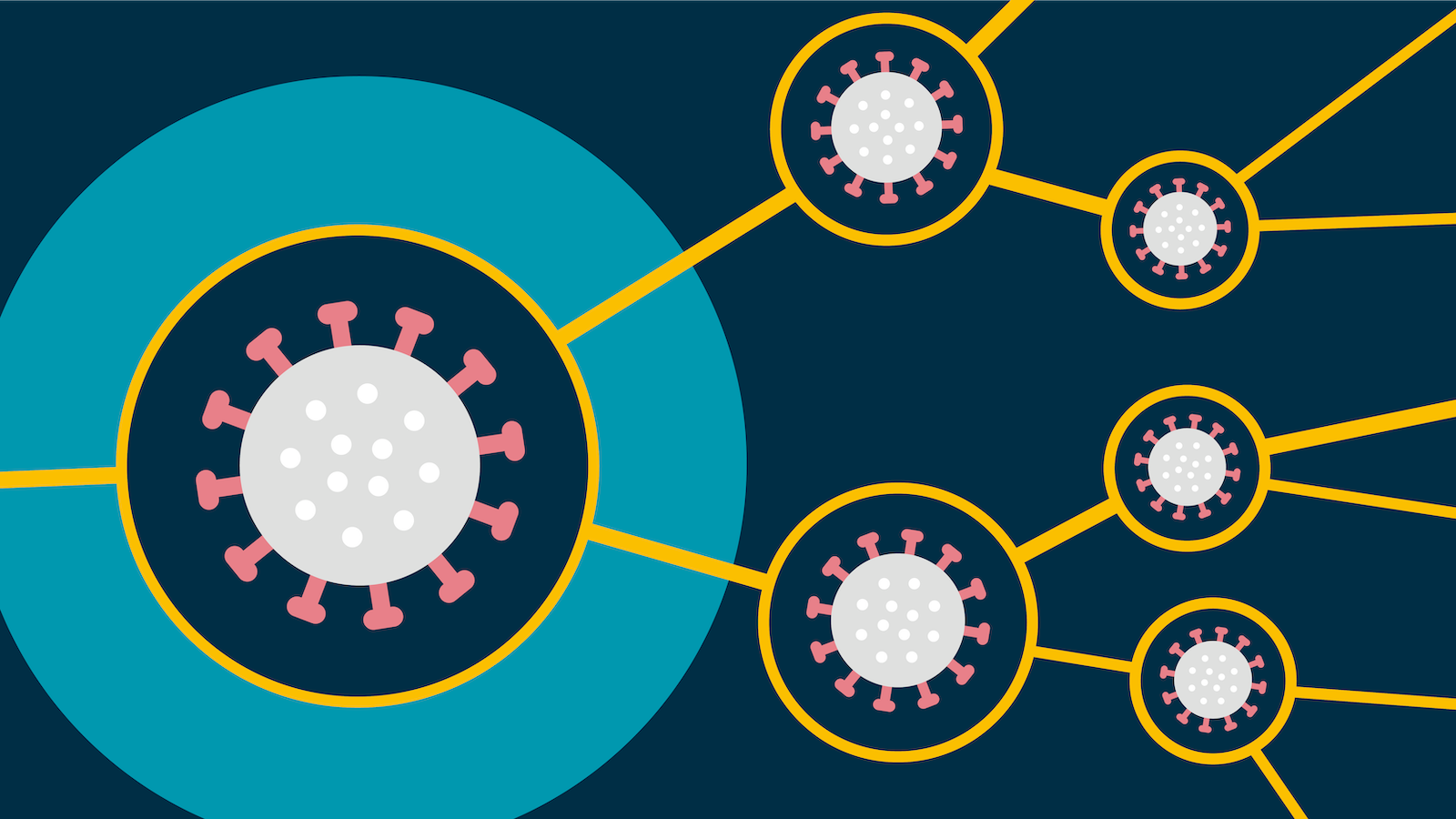
To spread, a virus needs to infect a host, replicate and produce lots of copies of itself.
When a virus replicates it doesn’t always manage to produce an exact copy of itself. This means that, over time, the virus may start to differ slightly in terms of its genetic sequence. Any changes to the viral genetic sequence during this process is known as a mutation and viruses with new mutations are sometimes called variants. Variants can differ by one or multiple mutations.
When a new variant has different functional properties to the original virus and becomes established in a population, it is sometimes referred to as a new strain of the virus. In short, all strains are variants, but not all variants are strains.
All viruses mutate. Most mutations are harmless and do not affect the properties of the virus. However, some mutations give the virus a selective advantage, increasing the likelihood that it will go on to infect another person.
Mutations which have a selective advantage could be ones which result in greater viral shedding – the release of infectious virus particles into the environment, for example when we talk, cough or sneeze – or they enable the virus to evade the body’s immune responses.
Potential consequences of new variants include:
-
change in transmissibility
-
difference in disease severity
-
ability to evade detection by viral diagnostic tests
-
reduced susceptibility to treatments
-
ability to evade natural or vaccine-induced immunity.
Why does the Covid-19 virus mutate?
Anna Mouser, Policy and Advocacy Lead, Vaccines: I wondered if you would describe for a layperson, a non-scientist, this issue of the virus evolving. How would you explain that to somebody without Biology A-Level or similar?
Sir Jeremy Farrar, OBE, Director of the Wellcome Trust: RNA viruses change a lot. HIV viruses are RNA viruses and influenza viruses are RNA viruses, and they mutate. They mutate randomly, there's no thinking behind it. It just happens. And then those mutations which give the virus an advantage, it can more easily go from me to you. It can transmit easier, it can pass to other people. Those viruses will become the dominant strains in a community. We've seen that in the UK, South Africa as well, where a mutation happened. It gave the virus an advantage. It was easier to transmit from one person to another and it became the dominant strain. What is more worrying is the fact that we now have people that have been infected and we're now starting to vaccinate people. Therefore, the virus that mutates in a way that escapes those vaccines or infections will also give those viruses an advantage and they will become the dominant strains. The best way of preventing that is to reduce the amount of viruses in the world, reduce the chances of mutations happening and reduce the chance of that variant having an advantage or becoming dominant. And the best way of doing that is to reduce transmission, make the vaccines available globally, and prevent those variants from happening. It's much easier to prevent than it is to respond to new variants coming into the population of viruses in the world.
Variants have the potential to make current treatments and vaccines less effective.
The influenza virus, which causes flu, is known to be a frequently mutating virus. Every flu season, we see several different influenza variants in circulation, which means that existing vaccines need to be updated so they are effective against the new variants.
Some individual mutations may reduce the virus’ sensitivity and vulnerability to human antibodies (part of the immune response) and could therefore make a vaccine or treatment less effective.
There have been many mutations of the virus (SARS-CoV-2) that causes Covid-19 since it was first identified in Wuhan.

A table of key Covid-19 variants (Alpha, Beta, Gamma, Delta and Omicron), when they emerged and why they are of concern.
Source: https://www.who.int/en/activities/tracking-SARS-CoV-2-variants/
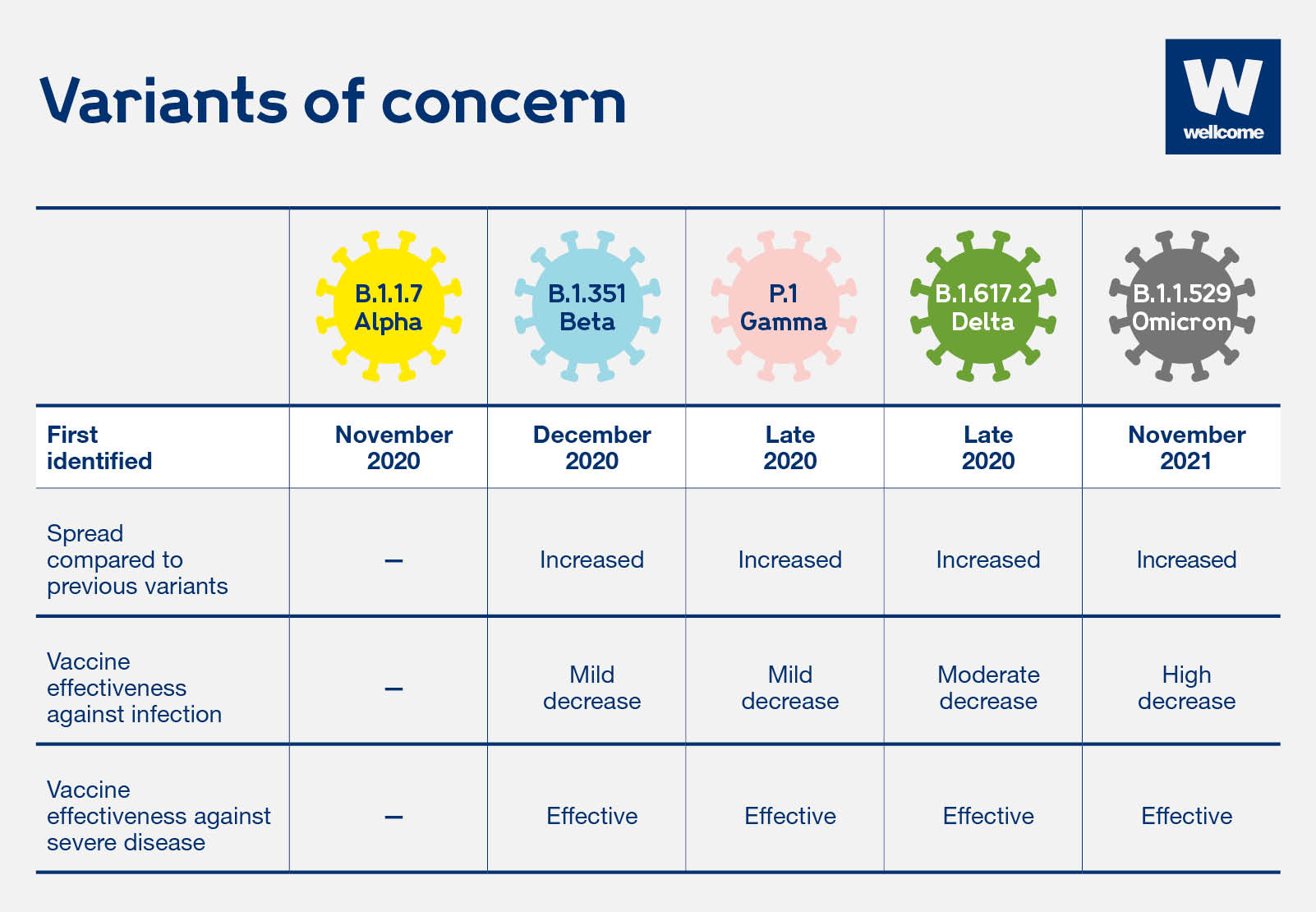
Currently, there are five variants of concern:
-
Alpha (formerly known as B.1.1.7 or 20I/501Y.V1, first identified in the UK)
Contains many mutations, several of which are on the spike protein (the protein used to enter our bodies cells). This variant is associated with increased transmissibility. -
Beta (formerly known as B.1.351 or 501Y.V2, first identified in South Africa)
Has the same mutations as Alpha (increased transmissibility) and also contains two other mutations which seem to make it harder for antibodies to bind to and destroy it. -
Gamma (formerly known as P1, first identified in a group of travellers from Brazil, who were tested at an airport in Japan)
Contains similar mutations to the B.1.351 variant. -
Delta (formerly known as B.1.617, first identified in India)
Preliminary studies show the Delta mutation spreads more easily than other variants and requires further study. -
Omicron (formerly known as B.1.1.529, first identified in South Africa)
This variant has a large number of mutations, some of which are concerning. Preliminary evidence suggests an increased risk of reinfection with this variant, as compared to other variants of concern.
How Covid-19 variants happen
All viruses naturally mutate. Sometimes a virus gets lucky and mutates in a way that helps it survive and spread more easily.
The virus that causes Covid-19 is no exception.
New variants have been spreading across the world.
They seem to transmit more easily. This could mean more people getting infected and more pressure on already stretched health services.
But we don't know yet how well existing treatments and vaccines will work against known and future variants.
To give the virus fewer opportunities to mutate, we need to cut transmission, increase the pace of research into Covid-19 treatments and vaccines and make them available fairly across the world.
Scientists need more funding for Covid-19 research.
Many Covid-19 vaccines target the spike protein. A virus that accumulates numerous mutations in the spike protein may be able to evade natural or vaccine-induced immunity.
There is ongoing research being conducted to test the efficacy of existing vaccine candidates against a range of variants. Vaccine developers may be able to update their candidates to make them more effective against new variants.
Early lab data suggests that the new variants – especially those first identified in South Africa and Brazil – may not respond to the first Covid-19 monoclonal antibodies (mAbs). Designed to bind to the spike protein of the virus, like a key in a lock, the mutations found in the variants mean that the key (mAbs) no longer fits the lock (spike protein). While this would be a disappointing setback, this class of treatments still holds great promise for Covid-19 and work is underway to develop combination and second-generation antibody treatments.
There are suggestions that the variants of concern are more prevalent in peoples’ noses and throats. This results in a higher viral load, making it easier for the virus to spread between hosts, continue to replicate, and potentially produce new mutations.
This is why it is important to continue to invest in development of a variety of vaccines and treatments to increase the chance of having tools that are effective against new variants.
Due to the potential for a mutation to change the properties of a virus, we need to monitor variants closely to determine if they pose a greater risk of transmission, severe disease or evasion of current interventions.
Since the 1980s we’ve been monitoring and sequencing influenza (flu) virus strains through global networks, to enable adaptation of the flu vaccine every year.
This is done through genetic sequencing of a virus, and the collection of epidemiological and clinical data. Scientists monitor any changes to a virus’ genome. Any concerning changes are reported and shared broadly so that public health interventions and policies can be adapted to limit the spread of a new variant nationally and worldwide.
Genomic surveillance – the way in which we track and monitor viruses – varies internationally. This is a concerning because we know that viruses – such as SARS-CoV-2 – do not respect geographical borders and new variants spread across countries. Lack of international genomic surveillance also leads to gaps in data and poses the risk of new harmful variants emerging and spreading undetected.
The GISAID Initiative promotes global rapid sharing of genetic sequencing and relevant epidemiological data associated with the Covid-19 pandemic. This data enables researchers and health authorities to determine if the new variant poses a greater risk of transmission, severe disease or evasion of current interventions. Collection of this data will also help target vaccines and therapeutics development and help monitor their impact when they are introduced.
On the flip side, if an increase in cases is noticed somewhere that cannot be explained or linked to a super-spreader event (for example, a workplace outbreak), health authorities may review the genetic surveillance data to look for mutations that could have caused the increase.
The more virus that is in circulation, the more opportunity it has to replicate and mutate, potentially producing new variants of concern. Suppression of the spread of the virus will reduce the number of new variants from emerging, while also protecting populations from spreading existing variants of a virus.
To limit spread, we should:
- follow public health interventions, such as social distancing and handwashing
- increase global capacity to monitor and sequence the virus to track and flag any significant changes
- prioritise equitable distribution of vaccines and treatments worldwide. If only a few countries have access to these, the virus will remain active, continue to spread and increase the risk of new variants emerging that evade current treatments and vaccines.
Why we need fair global vaccine allocation to end Covid-19
Sir Jeremy Farrar OBE, Director of the Wellcome Trust: The only way to bring the pandemic to a close and improve all of our lives is to make the vaccines available to everybody. So I would rather vaccinate some people in every country rather than vaccinate all people in some countries.
Vaccinating a lot of people in a small number of countries will not bring the pandemic to a close. And in fact it will encourage the development of new variants that may escape those very vaccines.
Governments, they're in very difficult positions. But what I would say to them that it is in their interests that we drive down transmission everywhere. If we don't, we will see new variants, we then go back into this awful pandemic of 2020. I think that is the message to policymakers and politicians the world over.
Leadership really matters. That what leadership needs to come out and say. Make the case for it and then make it happen and then I believe those leaders will be on the right side of history.
Special thanks to Hannah Chhoa-Howard (Graduate Trainee), Peter Hart (Research Adviser, Vaccines) and Deborah King (Vaccines Research Lead) for contributing to this article.
This article was originally published on 22 February 2021.
Delta, Omicron, Alpha. Covid-19 variants keep appearing. But this isn't surprising. All viruses naturally mutate and new variants of a virus are expected to occur over time. Epidemics Lead, Divya Shah, explains how variants happen, what they mean for vaccines and treatments and how we can prevent them.

